Yes the title is supposed to be “how scribes connect technology with humanity.” We thought it’s a clever play on words to “connect” them.
Idyllwild, CA – May 1, 2016 – by Kasaan Hammon
As technology continues to become a bigger and bigger part of modern patient care, providers and other experts struggle with the question, “Does health information technology dehumanize healthcare?” With HIPAA compliance at the forefront of administrators’ and providers’ minds, the balance between meeting requirements and meeting patient needs is at the heart of the matter. While technology strives to make healthcare more efficient, providers themselves strive to maintain the humanity in patient care.
The term “technology” was coined in 1829 by Jacob Bigelow, a physician at Massachusetts General Hospital who became an expert in botany while seeking to procure better medicines for his patients. Concerns about technology’s impact on humanity date back almost as far. When the stethoscope was introduced in the 1800’s, some doctors resisted its use because they felt it removed the intimacy of placing an ear to the patient’s chest. Those same concerns about care becoming more impersonal are echoed now as the introduction of EHR systems into the exam room shift a doctor’s focus from the patient to the computer screen.
Cultural analyst Sherry Turkle boils down the purpose of technology: “To take something complex and promise something simpler.” But she cautions that what we do with our technology defines who we are. Turkle examines the power of social media platforms like Facebook and Twitter to “force the feeling that someone is listening to us” in a world where we are “connected” in the technological sense and yet may feel more separate and alone than ever.1 In field experiments, researchers found that people who had conversations in the absence of mobile devices reported higher levels of empathetic concern, while those conversing in the presence of a device reported lower levels of empathy.2 In another study, mobile devices have negative effects on closeness, connection, and conversation quality, especially notable when individuals are engaging in personally meaningful topics.3
The translation of this effect to the doctor-patient setting is predictable as electronic devices enter the care setting. Patients’ desire for emotional connection, reassurance, and a healing touch from their caregivers as they communicate their health concerns is well documented and longstanding.4 When medical experts were asked by the Wall Street Journal to name the biggest factors to improving patient care, they agreed: eye contact, empathetic listening, and communication. Dr. Alex Lickerman, an internist who has taught medical students at University of Chicago, states, “Making the patient feel they have been heard may be one of the most important elements of doctoring. It’s not the actual time or lack of time people are complaining about – it’s how that time felt.”5The simple moments of direct attention, one-one-one eye contact, and touch are the key ingredients in a patient’s perception of a quality interaction.
Dr. John Sotos puts it this way: “Electronic health records demand communication time from the physician, and being legal documents, their need for attention can trump the patient’s need.” Researchers are asking what the impact is on patient satisfaction, and even the likelihood of malpractice complaints, when a doctor’s time is spent documenting and patients no longer feel heard when they seek medical advice. On average, a doctor will spend only 7-12 minutes with a patient and ask only 50% of all questions they have.6 Health columnist Roni Rabin writes, “By all accounts, short visits take a toll on the doctor-patient relationship. There is less of a dialogue between patient and doctor, increasing the odds patients will leave the office frustrated.”
But more listening and communication means even more to recall and more to document, hence the dilemma of where doctors’ time is spent. Dr. James Bailey wrote in the AMA’s Journal of Ethics, “The danger is that developers, lawmakers, researchers, and quality organizations, in their zeal to demonstrate “meaningful use” of health information technology (HIT), might establish design requirements for systems that mandate such extensive documentation at every visit that it eats up the already limited time doctors have to actually care for patients. The most common concerns about HIT have little to do with the technology itself, but everything to do with implementation.”7
Numerous studies have found that hospitals and clinics that bring on scribe services along with EHR implementation have been able to meet HIPAA guidelines while also improving patient satisfaction, doctor satisfaction, and efficiency in operations. Because scribes assume the tedious but essential task of properly and thoroughly documenting the patient visit, they free up physicians to spend more time focused directly on the patients. As Dr. Carol Cassella said in the Wall Street Journal panel, “Stop facing the computer. Look at your patients while you talk to them. Listen for more time than you talk. Body language can say more than words, but you’ll miss it if you aren’t looking.”5
Medical scribes, by making EHR documentation somewhat invisible and separate from the doctor-patient interaction, help ensure that documentation supports the purpose of the visit rather than becoming the centerpiece of it. While the fear may be that the technology will separate the doctor from the patient, when you add medical scribes to the equation, the doctor-patient interaction can actually be improved. Documentation is improved by use of the scribe, while the doctor has time to look, listen, communicate, and best serve the patient’s needs, thereby bridging the technology-humanity gap.
(1) Sherry Turkle, “Connected, but Alone?”, www.ted.com (February 2012); (2) Misra, Cheng, Genevie, & Yuan, “The iPhone Effect,” http://eab.sagepub.com (Sage, July 1, 2014); (3) Andrew Przybylski and Netta Weinstein, “Can You Connect with Me Now?”, http:// http://spr.sagepub.com/ (Sage, July 19, 2012); (4) Bailey JE. Asklepios: Ancient hero of medical caring (Ann Intern Med. 1996); and Wensing, Jung, Mainz, Olesen, Grol: A systematic review of the literature on patient priorities for general practice care (Soc Sci Med. 1998); (5) The Experts: “How to Improve Doctor-Patient Communication” (Wall Street Journal, April 12, 2013); (6) https://www.physiciancognition.com; (7) James e. Bailey, M.D, “Does Health Information Technology Dehumanize Health Care?” (AMA Journal of Ethics, March 2011)
 In-House Scribe SolutionsTake control of your medical scribe program
In-House Scribe SolutionsTake control of your medical scribe program Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization
Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization In-House Scribe SolutionsTake control of your medical scribe program
In-House Scribe SolutionsTake control of your medical scribe program In-house Scribe Program OverviewWith the ScribeConnect Scribe Management Platform you can have the best part of medical scribe’s EHR documentation help right in your organization.
In-house Scribe Program OverviewWith the ScribeConnect Scribe Management Platform you can have the best part of medical scribe’s EHR documentation help right in your organization. Overview and Key featuresMedical scribe management doesn’t have to be difficult, no matter what every other scribe providers tell you. The only SaaS medical scribe management platform is here for you.
Overview and Key featuresMedical scribe management doesn’t have to be difficult, no matter what every other scribe providers tell you. The only SaaS medical scribe management platform is here for you. for Healthcare OrganizationsFrom large hospital systems across urban centers, to small clinics operating in rural areas, our platform is designed to scale, grown, and accommodate your medical scribing needs.
for Healthcare OrganizationsFrom large hospital systems across urban centers, to small clinics operating in rural areas, our platform is designed to scale, grown, and accommodate your medical scribing needs. for Education InstitutesLooking for ways to offer your pre-med and pre-PA students more value? Or have a scribe training curriculum already in place and looking for a wider medical student audience? We can help.
for Education InstitutesLooking for ways to offer your pre-med and pre-PA students more value? Or have a scribe training curriculum already in place and looking for a wider medical student audience? We can help. for Scribe ApplicantsApply to medical scribe job openings across the country, and join a community of thousands of medical scribes. Access our comprehensive scribe training courses and more!
for Scribe ApplicantsApply to medical scribe job openings across the country, and join a community of thousands of medical scribes. Access our comprehensive scribe training courses and more! How to use our PlatformOur platform is simple to use, with robust features and powerful tools. Learn how to get the most out of our SaaS based platform with tips and tricks.
How to use our PlatformOur platform is simple to use, with robust features and powerful tools. Learn how to get the most out of our SaaS based platform with tips and tricks. Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization
Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization Full-Service Scribe Program OverviewWe hire, train, and manage your medical scribes so you don't have to.
Full-Service Scribe Program OverviewWe hire, train, and manage your medical scribes so you don't have to. Any provider, any time, anywhere.ScribeConnect has provided full-service, turn-key medical scribe programs for healthcare organizations large and small.
Any provider, any time, anywhere.ScribeConnect has provided full-service, turn-key medical scribe programs for healthcare organizations large and small. Frequently Asked QuestionsHere are some frequently asked questions that may help you decide whether or not a medical scribe program is right for you.
Frequently Asked QuestionsHere are some frequently asked questions that may help you decide whether or not a medical scribe program is right for you. Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence.
Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence. Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence.
Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence. Solutions For Your Healthcare OrganizationEase your documentation load, keep your providers happy, and improve your revenue cycle with ScribeConnect Medical Scribe Solutions. Designed for Healthcare Networks, Clinics, Hospitals, Emergency Departments, and Practice Management Groups
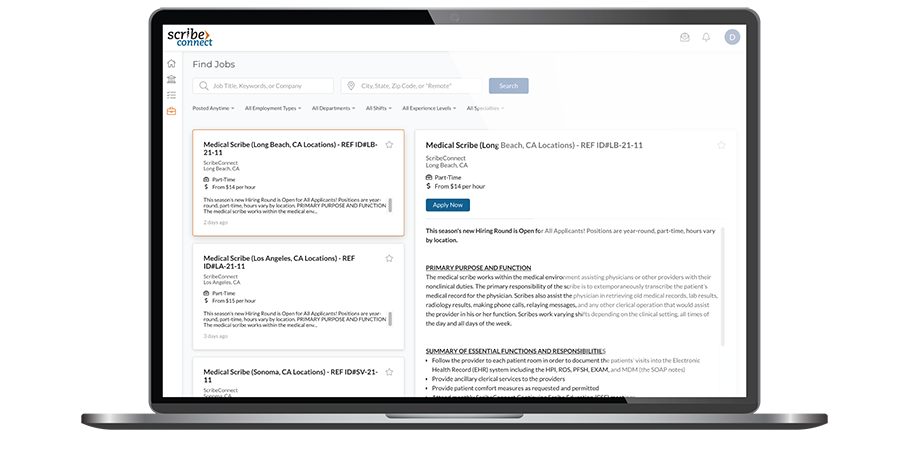
Solutions For Your Healthcare OrganizationEase your documentation load, keep your providers happy, and improve your revenue cycle with ScribeConnect Medical Scribe Solutions. Designed for Healthcare Networks, Clinics, Hospitals, Emergency Departments, and Practice Management Groups Post A Job & Track ApplicantsWhether you're hiring one scribe, or an entire team or teams of scribes, we have America's largest dedicated medical scribe job board. Post, manage, and HIRE the most qualified scribes.
Post A Job & Track ApplicantsWhether you're hiring one scribe, or an entire team or teams of scribes, we have America's largest dedicated medical scribe job board. Post, manage, and HIRE the most qualified scribes. Course CatalogOur industry-leading, academically-based, professional Medical Scribe Training Courses (MSTCs) are designed for a range of topics, from general and continuing scribe training to in-depth specialty-specific courses.
Course CatalogOur industry-leading, academically-based, professional Medical Scribe Training Courses (MSTCs) are designed for a range of topics, from general and continuing scribe training to in-depth specialty-specific courses. Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program.
Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program. Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program.
Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program. Academic PartnershipsSee what a partnership with ScribeConnect can do for your department and institution.
Academic PartnershipsSee what a partnership with ScribeConnect can do for your department and institution. Learn About Our Collegiate CoursesLearn about our academically-rigorous certificate courses that have been developed for the college student and how they can complement & expand your program's offerings.
Learn About Our Collegiate CoursesLearn about our academically-rigorous certificate courses that have been developed for the college student and how they can complement & expand your program's offerings. Financial Partnership ProgramSee how our financial partnership program can provide your institution with a new income stream in an extremely fast-growing, emerging, and competitive industry.
Financial Partnership ProgramSee how our financial partnership program can provide your institution with a new income stream in an extremely fast-growing, emerging, and competitive industry. ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level.
ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level. ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level.
ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level. What We Can Do For YOU?ScribeConnect has built a rich legacy of helping pre-medical professionals launch their careers. Now we're providing more powerful tools than ever before to help you win. See how.
What We Can Do For YOU?ScribeConnect has built a rich legacy of helping pre-medical professionals launch their careers. Now we're providing more powerful tools than ever before to help you win. See how. Find JobsSearch our job board and apply to jobs in your area. Apply to work directly with ScribeConnect at one of our locations or apply directly to one of our partners.
Find JobsSearch our job board and apply to jobs in your area. Apply to work directly with ScribeConnect at one of our locations or apply directly to one of our partners. Course CatalogPosition yourself above the competition when you get certified through our rigorous Medical Scribe Training Courses (MSTCs). You'll be prepared and equipped to work as a scribe in the medical setting of your choice.
Course CatalogPosition yourself above the competition when you get certified through our rigorous Medical Scribe Training Courses (MSTCs). You'll be prepared and equipped to work as a scribe in the medical setting of your choice.