In today’s healthcare setting, EHR transition is in the air.
Idyllwild, CA – October 1, 2016 – by Kasaan Hammon
As the world of medicine integrates more and more new technology into patient care, healthcare providers manage the transition from paper charts to electronic health records (EHRs). Developed in an effort to improve communication and quality of care as patients transition from one setting to another, the implementation of electronic medical recordss has left doctors themselves in transition. And as the many sayings go, change is inevitable, change is good, and change can be hard. As doctors and administrators face the challenge of electronic transitioning head-on, perhaps the best way to navigate these changes is to explore three basic questions: Why is change needed? What change is in order? How best can this change be accomplished?
Talk to an Implementation Specialist about Building Your Scribe Program
Looking first at why change has become necessary in the modern healthcare setting, the reasons are ample. When surveyed, patients and their caregivers have often reported experiencing quality problems when they encounter the healthcare system. Surveys by the National Partnership for Women & Families found that there are two very consistent negative points when interacting with the healthcare system: lack of communication and lack of coordination.(1) Thus, consolidating health information via electronic records ultimately seeks to facilitate both better communication and coordination of care.
From the physician’s perspective, paper charting is time-consuming, taking time away from patient care. It can also be cumbersome to communicate patient records between care settings and potentially inefficient with respect to billing. Due to high demands for physician productivity, charting is typically done after patients are seen, not real-time, leaving a wide window for chart omissions and errors, as well as downgraded billing and potential for malpractice lawsuits due to such omissions and errors.
The proposed benefits of health information technology (HIT) with respect to efficiency and overall quality of care include eliminating paper medical records and expanding the exchange of health information, avoiding duplicate or unnecessary diagnostic tests and radiological services, promoting cost‐effective use of prescription drugs and avoiding adverse drug events, improving nurse and physician productivity, and reducing the length of hospital stays.(2) Transitioning to an EHR establishes the communication record and network necessary to maintain and streamline patient care from provider to provider, clinical setting to clinical setting.
The implementation of electronic health records as mandated by the HITECH Act incentivizes a smooth and expedient transition from paper to electronic records. However, in many instances, this requires physicians to change the way they practice medicine, and radical changes require organizational commitment along with financial investment.(2) Practices may lose up to 50% of patient volume, and therefore revenue, as they convert to an electronic record. These considerations have left many doctors resistant to change and overwhelmed by the added burden of having to navigate an entirely electronic recordkeeping system while maintaining an entirely human quality of compassionate care. It also calls for examination of organizational structures and possible restructuring.
A broader look at how organizations view and approach change can be helpful. Due to institutional preconceptions about change, change can be more difficult, expensive, and slower than it needs be. The management of change in complex systems, however, does require an understanding of the significance of those changes as well as their consequences in terms of performance and safety. Certain industry segments have developed cultural beliefs that in part are focused on constraining change until significant evidence indicates that unintended consequences will not occur. The two sets of perceptions—the desire for timely incorporation of change, and caution in the face of its possible effects—create a significant tension between those charged with the integration of new technology capabilities and those who feel accountable for the consequences of such technology incorporation.(3)
Committees on accelerating technology transition stress the importance of creating a culture for innovation and speedy technology transition. Individuals and subcultures within an organization play a vital role in determining the success or failure of technology transition. The successful transition of new technology depends on the ability of organizational leaders to narrow the focus to what technologies should be implemented, properly assign roles within the organization to best utilize the new technology, and find champions who will remove barriers, garner support, and ensure successful implementation and acceptance.
Virginia Martin, a Medical Economics consultant and president of Healthcare Consulting Associates of NW Ohio, Inc., advises the following steps in facing the specific challenge of electronic healthcare record transitioning: Make a plan; define your team; use available resources; choose a vendor; set pre-implementation, implementation, and post-implementation projects.(4) Defining the best team in light of EHR implementation requires examination of organizational roles within the practice, including which staff will need training on the documentation system and whether implementing medical scribes to handle health record documentation may be a better use of staff and resources.
Though facing these challenges can be daunting, there are companies which specifically provide transition services to help providers navigate the process. Companies like ScribeConnect, a national scribe service provider, in addition to building and managing full service scribe programs, provide EHR transition assistance, including assistance with identifying the right electronic health record provider, customizing and integrating the system to the specific needs of the practice or clinical setting, training employees on the system, and development of templates and macros specific to the practice. Services such as these during the “go-live” period can significantly reduce any productivity loss that would normally be associated with EHR transitions.
While the changes called for in healthcare today may be technological, the methods to deal with these changes are fundamentally human: reflecting on why change is needed; preparing mentally and emotionally for change; relying on good resources to ease the transition process; and ultimately, embracing the benefits change will bring.
(1) Lake Media Poll Report, “Effects of Poor Communication and Coordination in Health Care System,” Lake Research Partners for the National Partnership for Women & Families, 2010; (2) Health Information Technology Work Group, “Improving Transitions of Care with Health Information Technology,” National Transitions of Care Coalition, December 2010; (3) National Research Council of the National Academies, “Accelerating Technology Transition,” National Academies Press, 2004; (4) Virginia Martin, “Easing the Transition to Electronic Health Records,” Medical Economics, December 2010.
 In-House Scribe SolutionsTake control of your medical scribe program
In-House Scribe SolutionsTake control of your medical scribe program Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization
Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization In-House Scribe SolutionsTake control of your medical scribe program
In-House Scribe SolutionsTake control of your medical scribe program In-house Scribe Program OverviewWith the ScribeConnect Scribe Management Platform you can have the best part of medical scribe’s EHR documentation help right in your organization.
In-house Scribe Program OverviewWith the ScribeConnect Scribe Management Platform you can have the best part of medical scribe’s EHR documentation help right in your organization. Overview and Key featuresMedical scribe management doesn’t have to be difficult, no matter what every other scribe providers tell you. The only SaaS medical scribe management platform is here for you.
Overview and Key featuresMedical scribe management doesn’t have to be difficult, no matter what every other scribe providers tell you. The only SaaS medical scribe management platform is here for you. for Healthcare OrganizationsFrom large hospital systems across urban centers, to small clinics operating in rural areas, our platform is designed to scale, grown, and accommodate your medical scribing needs.
for Healthcare OrganizationsFrom large hospital systems across urban centers, to small clinics operating in rural areas, our platform is designed to scale, grown, and accommodate your medical scribing needs. for Education InstitutesLooking for ways to offer your pre-med and pre-PA students more value? Or have a scribe training curriculum already in place and looking for a wider medical student audience? We can help.
for Education InstitutesLooking for ways to offer your pre-med and pre-PA students more value? Or have a scribe training curriculum already in place and looking for a wider medical student audience? We can help. for Scribe ApplicantsApply to medical scribe job openings across the country, and join a community of thousands of medical scribes. Access our comprehensive scribe training courses and more!
for Scribe ApplicantsApply to medical scribe job openings across the country, and join a community of thousands of medical scribes. Access our comprehensive scribe training courses and more! How to use our PlatformOur platform is simple to use, with robust features and powerful tools. Learn how to get the most out of our SaaS based platform with tips and tricks.
How to use our PlatformOur platform is simple to use, with robust features and powerful tools. Learn how to get the most out of our SaaS based platform with tips and tricks. Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization
Contracted Full-Service Scribe SolutionsWe Build a Turn-Key Scribe Program For Your Organization Full-Service Scribe Program OverviewWe hire, train, and manage your medical scribes so you don't have to.
Full-Service Scribe Program OverviewWe hire, train, and manage your medical scribes so you don't have to. Any provider, any time, anywhere.ScribeConnect has provided full-service, turn-key medical scribe programs for healthcare organizations large and small.
Any provider, any time, anywhere.ScribeConnect has provided full-service, turn-key medical scribe programs for healthcare organizations large and small. Frequently Asked QuestionsHere are some frequently asked questions that may help you decide whether or not a medical scribe program is right for you.
Frequently Asked QuestionsHere are some frequently asked questions that may help you decide whether or not a medical scribe program is right for you. Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence.
Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence. Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence.
Healthcare OrganizationsOur platform empowers your organization with intuitive tools to recruit, track applicants, train & certify scribes, and manage teams. Build and grow a strong and dynamic scribe program of any size with confidence. Solutions For Your Healthcare OrganizationEase your documentation load, keep your providers happy, and improve your revenue cycle with ScribeConnect Medical Scribe Solutions. Designed for Healthcare Networks, Clinics, Hospitals, Emergency Departments, and Practice Management Groups
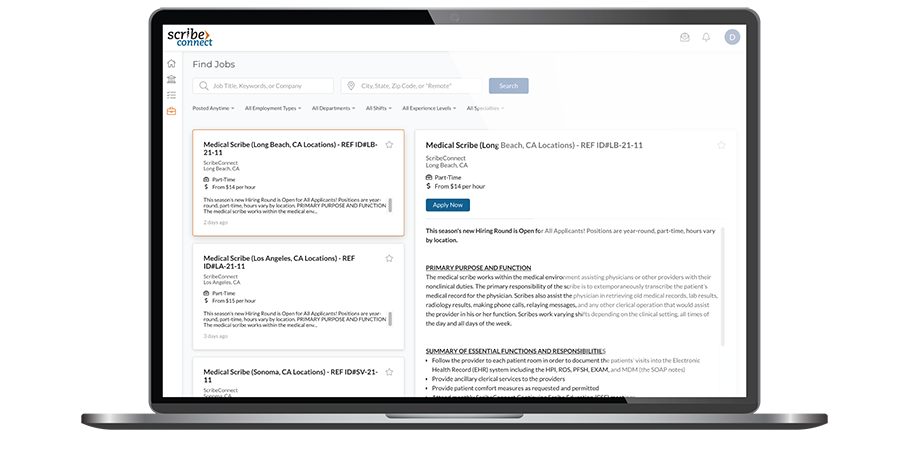
Solutions For Your Healthcare OrganizationEase your documentation load, keep your providers happy, and improve your revenue cycle with ScribeConnect Medical Scribe Solutions. Designed for Healthcare Networks, Clinics, Hospitals, Emergency Departments, and Practice Management Groups Post A Job & Track ApplicantsWhether you're hiring one scribe, or an entire team or teams of scribes, we have America's largest dedicated medical scribe job board. Post, manage, and HIRE the most qualified scribes.
Post A Job & Track ApplicantsWhether you're hiring one scribe, or an entire team or teams of scribes, we have America's largest dedicated medical scribe job board. Post, manage, and HIRE the most qualified scribes. Course CatalogOur industry-leading, academically-based, professional Medical Scribe Training Courses (MSTCs) are designed for a range of topics, from general and continuing scribe training to in-depth specialty-specific courses.
Course CatalogOur industry-leading, academically-based, professional Medical Scribe Training Courses (MSTCs) are designed for a range of topics, from general and continuing scribe training to in-depth specialty-specific courses. Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program.
Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program. Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program.
Educational InstitutionsFrom enrollment to alumni services, ScribeConnect’s platform can be your powerhouse medical scribe training and certification program. Academic PartnershipsSee what a partnership with ScribeConnect can do for your department and institution.
Academic PartnershipsSee what a partnership with ScribeConnect can do for your department and institution. Learn About Our Collegiate CoursesLearn about our academically-rigorous certificate courses that have been developed for the college student and how they can complement & expand your program's offerings.
Learn About Our Collegiate CoursesLearn about our academically-rigorous certificate courses that have been developed for the college student and how they can complement & expand your program's offerings. Financial Partnership ProgramSee how our financial partnership program can provide your institution with a new income stream in an extremely fast-growing, emerging, and competitive industry.
Financial Partnership ProgramSee how our financial partnership program can provide your institution with a new income stream in an extremely fast-growing, emerging, and competitive industry. ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level.
ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level. ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level.
ScribesAspiring scribes begin their education and path to employment here, while experienced scribes can learn valuable new skills and specialty-specific knowledge to take it to the next level. What We Can Do For YOU?ScribeConnect has built a rich legacy of helping pre-medical professionals launch their careers. Now we're providing more powerful tools than ever before to help you win. See how.
What We Can Do For YOU?ScribeConnect has built a rich legacy of helping pre-medical professionals launch their careers. Now we're providing more powerful tools than ever before to help you win. See how. Find JobsSearch our job board and apply to jobs in your area. Apply to work directly with ScribeConnect at one of our locations or apply directly to one of our partners.
Find JobsSearch our job board and apply to jobs in your area. Apply to work directly with ScribeConnect at one of our locations or apply directly to one of our partners. Course CatalogPosition yourself above the competition when you get certified through our rigorous Medical Scribe Training Courses (MSTCs). You'll be prepared and equipped to work as a scribe in the medical setting of your choice.
Course CatalogPosition yourself above the competition when you get certified through our rigorous Medical Scribe Training Courses (MSTCs). You'll be prepared and equipped to work as a scribe in the medical setting of your choice.